Introduction
Back
Pediatric tuberculosis (TB) presents significant diagnostic challenges, particularly in low-resource settings where healthcare infrastructure is limited. According to global health experts, children are a vulnerable population often overlooked in TB diagnosis, leading to high rates of underreporting and undiagnosed cases. This issue is further compounded by the non-specific clinical and radiological presentation of TB in children, making diagnosis complex. However, artificial intelligence (AI) is emerging as a transformative tool to bridge these gaps in paediatric TB screening and diagnosis, offering the potential to improve diagnostic accuracy and streamline treatment pathways.
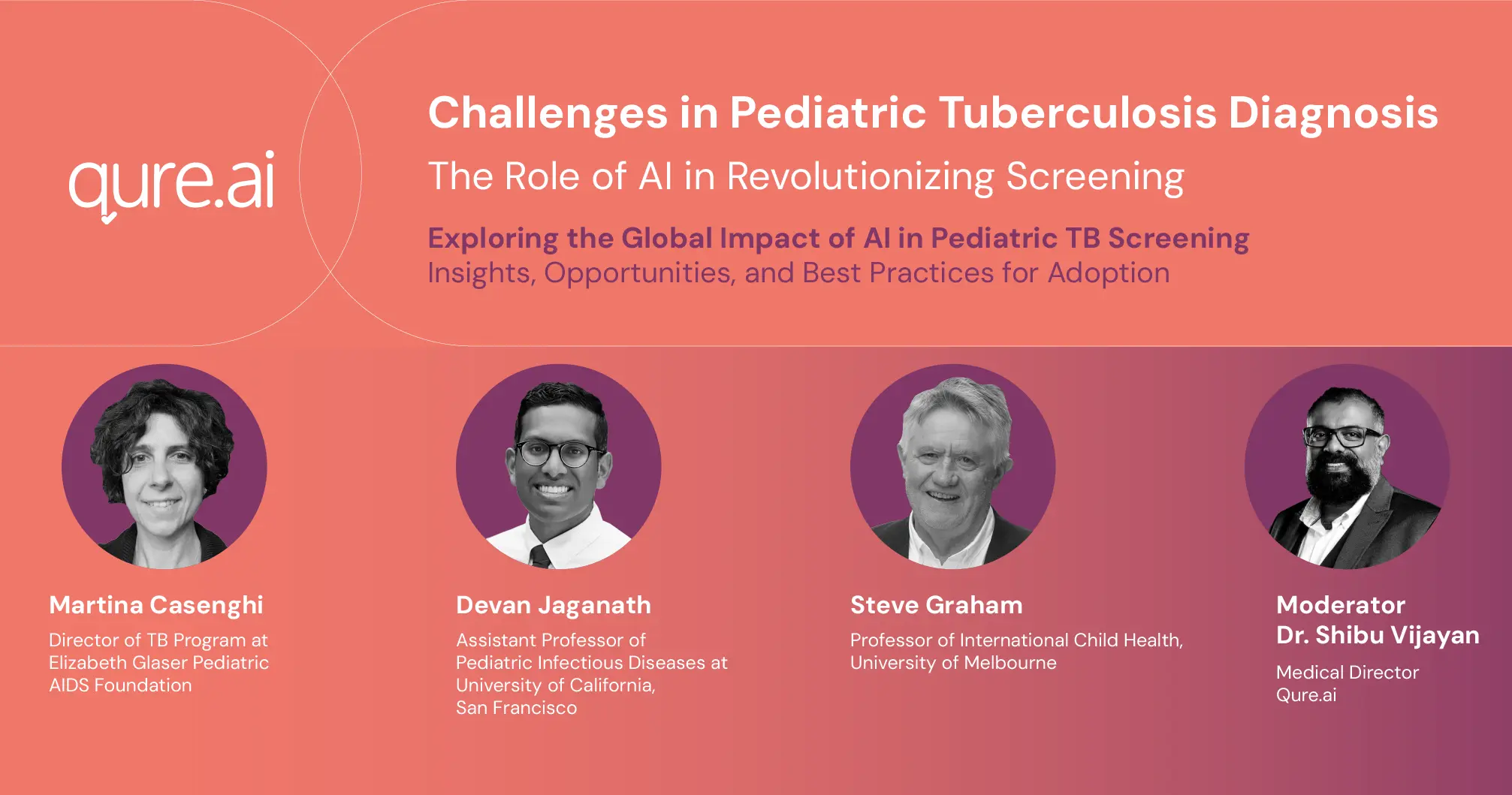
This article deep-dives into the insights shared during a webinar held on September 12, featuring prominent experts in paediatric TB, and explores the role of AI in addressing these diagnostic challenges.
Current Challenges in Pediatric TB Diagnosis
Professor Steve Graham of the University of Melbourne underscored the significant gap in TB diagnosis among children. Globally, approximately 72.5% of children under five who are in contact with TB patients remain undiagnosed. In the age group of 5-14, only 44.6% of the cases are reported. These alarming statistics highlight the need for innovative diagnostic solutions, particularly in underserved regions.
Graham noted that TB diagnosis in young children is particularly challenging due to their non-specific clinical presentations, which often mimic other diseases like pneumonia or malnutrition. The difficulty of interpreting chest X-rays in this population further complicates the process. Only a minority of paediatric TB cases can be confirmed bacteriologically, leaving healthcare workers to rely on clinical judgment, which can be subjective and error-prone.
Graham also advocated for the decentralisation of TB services, a strategy that has been effective in bringing diagnosis and treatment closer to communities. However, decentralisation alone is not enough. There is a pressing need for an algorithmic approach to diagnosing TB, especially when interpreting chest X-rays. AI has the potential to enhance diagnostic confidence by distinguishing between normal and abnormal X-ray findings and identifying specific features indicative of TB.
The Role of AI in Pediatric TB Screening
Dr. Devan Jaganath from the University of California, San Francisco, discussed the potential of AI in paediatric TB diagnosis, particularly in overcoming the limitations of traditional diagnostic methods. AI-powered tools can analyse clinical data, biomarkers, and imaging results to improve diagnostic accuracy. However, Jaganath stressed that the current infrastructure is insufficient to fully implement AI in paediatric TB diagnosis. Developing AI tools tailored to the needs of younger patients is crucial, and healthcare providers must collaborate with developers to ensure that the necessary data is available to train AI systems effectively.
AI’s ability to assist in diagnosing complex cases of paediatric TB is particularly promising. For example, AI can help detect lymphadenopathy, a common symptom of TB, on chest X-rays. However, as Graham pointed out, many children with TB may not present with easily diagnosable symptoms, underscoring the need for AI tools that can handle a wide range of clinical scenarios.
Challenges in Implementation
Dr. Martina Casenghi from the Elizabeth Glaser Pediatric AIDS Foundation shared her experiences implementing TB diagnostic programs across ten countries. Access to chest X-rays was a significant challenge, particularly in African nations, where infrastructure gaps and the cost of diagnostic tools limited availability. While India had relatively better access to X-ray technology, training healthcare workers to accurately interpret X-rays remained a hurdle. Casenghi emphasised the need for affordable and scalable AI solutions that can be easily adopted in low-resource settings.
One of the key challenges in AI adoption is the disparity in healthcare infrastructure between countries. Casenghi stressed the importance of ensuring that AI tools are integrated into existing health systems in a way that enhances rather than complicates the diagnostic process. Additionally, funding remains a major obstacle, with global health organisations often prioritising adult TB over paediatric cases. This prioritisation must shift to ensure that children receive the attention they deserve.
Advances in Treatment and Precision Medicine
Both Graham and Jaganath discussed the advances in TB treatment, particularly the move toward precision medicine. AI has the potential to assist in selecting appropriate treatment regimens, whether it’s the shorter four-month regimen or the standard six-month treatment. As Jaganath pointed out, confidently diagnosing TB and determining its severity are crucial steps in choosing the most effective treatment. AI can play a pivotal role in these decisions by analysing clinical data and helping healthcare providers make more informed choices.
However, the road to fully integrating AI into TB treatment is not without challenges. Graham noted that while computer-aided diagnosis (CAD) is currently used as a diagnostic tool in adults, it has not yet been widely adopted for children. The question remains whether AI should be used as a screening tool or primarily to support diagnosis. This distinction is critical as countries look to reduce TB transmission rates through early and accurate detection.
The Path Forward: Democratising Pediatric TB Diagnosis
The panelists agreed that democratising access to paediatric TB diagnosis is essential for reducing the global TB burden. AI has the potential to play a transformative role in this effort, but its success depends on several factors: the availability of infrastructure, training for healthcare workers, and the development of AI tools tailored to paediatric needs. Moreover, governments and healthcare organisations must prioritise funding for paediatric TB programs and ensure that AI is integrated into national TB strategies.
To achieve these goals, community engagement is vital. Graham highlighted the importance of educating parents and caregivers about the importance of TB screening for their children. Traditional methods, such as using flipcharts and engaging TB survivors to educate communities in their local languages, have proven effective in raising awareness and encouraging early detection.
Conclusion
Pediatric TB remains a significant global health challenge, but AI offers a promising solution to improve diagnosis and treatment. By leveraging AI’s ability to analyse complex clinical data and interpret chest X-rays with greater accuracy, healthcare providers can bridge the diagnostic gap and ensure that more children receive timely and appropriate treatment. However, the successful adoption of AI in paediatric TB care will require a concerted effort from governments, healthcare providers, and developers to address infrastructure gaps, train healthcare workers, and prioritise funding for paediatric TB programs. Through collaboration and innovation, AI has the potential to transform paediatric TB care and bring us closer to eliminating this preventable disease.